Laser Therapy For Carpal Tunnel Syndrome Webinar Transcription
 Certain infections that can cause swelling and edema can also be problematic. And inflammatory conditions like rheumatoid arthritis, local tendonitis and gout may also cause carpal tunnel syndrome. And again, anything that increases canal volume. So we know that it tends to be a bit more common during pregnancy as a woman’s retaining fluid. But of course, that’s more of a temporary type of condition.
Being obese, hypertension, edema, this is secondary to repetitive use. These are all possible ways of increasing the canal volume. Certain metabolic conditions, it tends to be more frequent in, for example, diabetes and hypothyroidism as well.
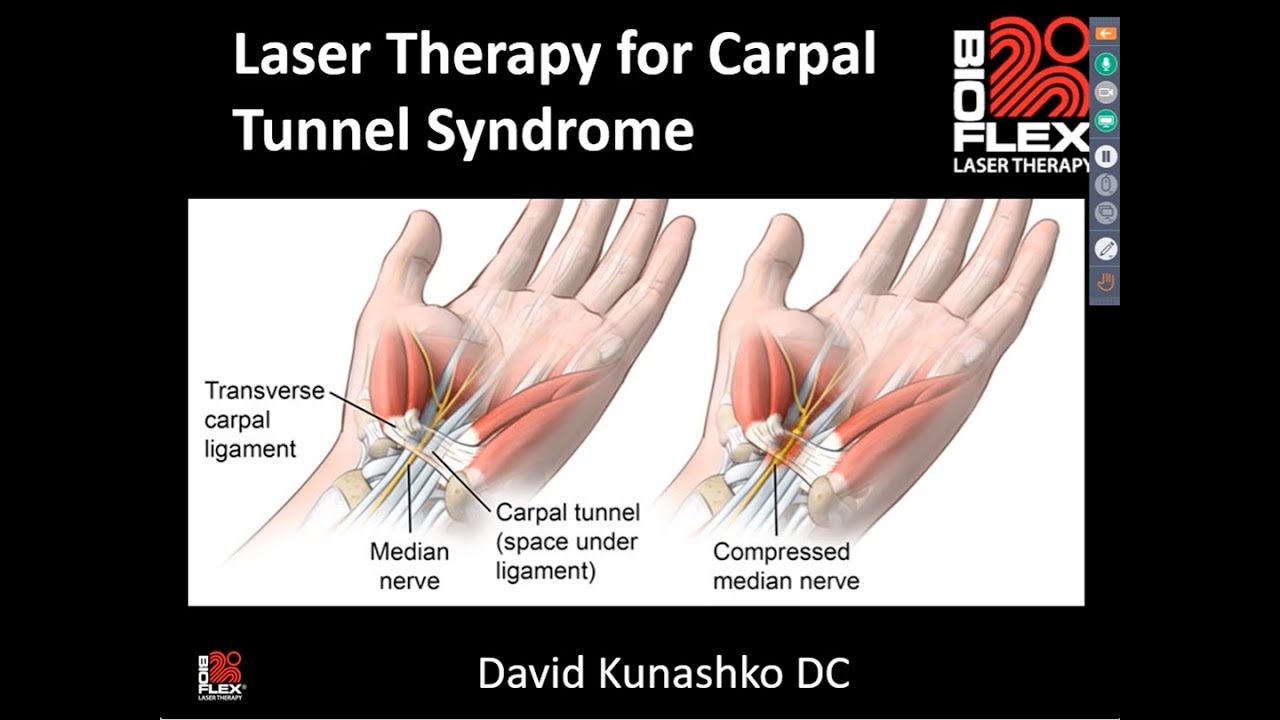
As far as symptoms go, initially they tend to be more nocturnal or in the evening during the sleep, often waking the patient up. This is usually pain and paresthesia and the distribution of median nerve as shown in the diagram on the right, which includes the Palmer aspect of the thumb, index and middle fingers and the radial half of the ring finger.
In the early stages, symptoms can vary widely, they can even localize to the entire hand or the wrist to other areas or radiate around the forearm much. Rarely does it radiate past proximal to the elbow and into the shoulder, but that can happen. So sometimes a patient will talk about some signs and symptoms or especially pain proximal to the wrist and that can occur in CTS, so just be aware of that as well. Of course, you should be also looking for double crush syndrome or other areas that may also be causing similar symptoms. So patients often awaken with these symptoms, they’ll try to shake it out, kind of get rid of those symptoms during the evening. This is called the flick sign and if this is occurring in patients, it tends to be 93% sensitive and 96% specific for the diagnosis of carpal tunnel syndrome.
Since sensory fibers tend to be more susceptible to compression than motor fibers, generally speaking it’s a paresthesia that’s predominant and pain as opposed to motor symptoms. However, as this progresses you then start to get issues with the motor fibers that will lead to weakness of an eventual atrophy in late stages and more severe cases of carpal tunnel syndrome.
One interesting note I discovered I wasn’t even aware of this is that in late stages actually you can get disappearance of pain. That can be a late finding that implies a permanent sensory loss and obviously a very ominous sign as far as the pathophysiology goes. So as a review you’re going to see sensory disturbances specifically in the median nerve distribution. Check during your examination for any motor loss or atrophy or weakness of the thumb abduction. So those are important screening tests as well as diagnostic tests I’m sure you’re all familiar with, like phalen’s, where you hold the wrist and unilaterally, bilaterally, when you have the patient hold for at least a minute or so and looking for the symptoms to be aggravated or reappear.
Tinel sign, tapping over the median nerve and again looking for a positive response with respect to increase in tingling or paresthesia in the median nerve distribution. There’s a few other tests including compression and distribution between specific points. That’s the SW monofilament or vibration sensitivity. And you can see here that when you’re doing diagnostic measures there’s sensitivity which correctly identifies patients with the actual condition. So in this case a positive test for carpal tunnel or a specificity which correctly identifies those without the disease.
So if you’re looking at these types of testing, you can see that Phalens and tinel don’t have a great sensitivity. However, tinel is quite specific for patients that don’t have the condition, whereas other tests like true compression or sensory testing has a bit better sensitivity, especially vibration sense.
Certain infections that can cause swelling and edema can also be problematic. And inflammatory conditions like rheumatoid arthritis, local tendonitis and gout may also cause carpal tunnel syndrome. And again, anything that increases canal volume. So we know that it tends to be a bit more common during pregnancy as a woman’s retaining fluid. But of course, that’s more of a temporary type of condition.
Being obese, hypertension, edema, this is secondary to repetitive use. These are all possible ways of increasing the canal volume. Certain metabolic conditions, it tends to be more frequent in, for example, diabetes and hypothyroidism as well.
As far as symptoms go, initially they tend to be more nocturnal or in the evening during the sleep, often waking the patient up. This is usually pain and paresthesia and the distribution of median nerve as shown in the diagram on the right, which includes the Palmer aspect of the thumb, index and middle fingers and the radial half of the ring finger.
In the early stages, symptoms can vary widely, they can even localize to the entire hand or the wrist to other areas or radiate around the forearm much. Rarely does it radiate past proximal to the elbow and into the shoulder, but that can happen. So sometimes a patient will talk about some signs and symptoms or especially pain proximal to the wrist and that can occur in CTS, so just be aware of that as well. Of course, you should be also looking for double crush syndrome or other areas that may also be causing similar symptoms. So patients often awaken with these symptoms, they’ll try to shake it out, kind of get rid of those symptoms during the evening. This is called the flick sign and if this is occurring in patients, it tends to be 93% sensitive and 96% specific for the diagnosis of carpal tunnel syndrome.
Since sensory fibers tend to be more susceptible to compression than motor fibers, generally speaking it’s a paresthesia that’s predominant and pain as opposed to motor symptoms. However, as this progresses you then start to get issues with the motor fibers that will lead to weakness of an eventual atrophy in late stages and more severe cases of carpal tunnel syndrome.
One interesting note I discovered I wasn’t even aware of this is that in late stages actually you can get disappearance of pain. That can be a late finding that implies a permanent sensory loss and obviously a very ominous sign as far as the pathophysiology goes. So as a review you’re going to see sensory disturbances specifically in the median nerve distribution. Check during your examination for any motor loss or atrophy or weakness of the thumb abduction. So those are important screening tests as well as diagnostic tests I’m sure you’re all familiar with, like phalen’s, where you hold the wrist and unilaterally, bilaterally, when you have the patient hold for at least a minute or so and looking for the symptoms to be aggravated or reappear.
Tinel sign, tapping over the median nerve and again looking for a positive response with respect to increase in tingling or paresthesia in the median nerve distribution. There’s a few other tests including compression and distribution between specific points. That’s the SW monofilament or vibration sensitivity. And you can see here that when you’re doing diagnostic measures there’s sensitivity which correctly identifies patients with the actual condition. So in this case a positive test for carpal tunnel or a specificity which correctly identifies those without the disease.
So if you’re looking at these types of testing, you can see that Phalens and tinel don’t have a great sensitivity. However, tinel is quite specific for patients that don’t have the condition, whereas other tests like true compression or sensory testing has a bit better sensitivity, especially vibration sense.
 Okay, let’s talk a bit about some of the research that I’ve come across with respect to LLLT and carpal tunnel syndrome. This paper was a randomized control trial put out in 2014. It was a double blinded randomized trial. 79 patients with mild to moderate carpal tunnel syndrome.
A lot of the research refers to mild to moderate cases. You will find that it is recommended to treat these cases with LT. However, if it’s a severe case, then chances are they won’t respond very well. And those are cases more that require surgical intervention or more serious types of interventions. This trial used 780 infrared light, 30 milliwatts and a continuous wave.
They treated four points with a contact technique. Each point they held for 90 seconds. So, quite a long time frame. They treated five times a week, once per day for two weeks. So ten treatments in total then every other day for three weeks, for a total of 20 treatments.
Okay, so they were looking at visual analog scale, they were looking at the tinel sign, and they also did neurometrics testing as well for a nerve conduction test. Neurometrics, we use this in our clinic as well too, as a superficial EMG, quite easy to do, gets a result very quickly, almost instantaneously. So if you have the ability to do this or test for it, it really does give objective measurements, pre and post treatment to really get a gauge to see if the motor fibers and the sensory fibers are improving with time and treatment. So they observed that there was significant reduction in pain in this particular trial. There was a reduction in the percentage of patients with the positive tinel sign. And they also found a shortening of the sensory and motor latency with respect to the nerve conduction examination. So overall, they found it quite useful to use LLT with respect to carpal tunnel syndrome.
Another paper published in 2016, so fairly recently they looked at, it was a metal analysis, essentially looking at seven randomized clinical trials. 261 in the control group and 270 in the laser treated group. They concluded that there was improved hand grip, improved bas scale pain, as well as snap testing with respect to functionality of the carpal tunnel.
After three months, a follow up for mild to moderate carpal tunnel syndrome. Again, make note of mild to moderate cases. They did recommend more high quality studies to be done, as most metaanalysis studies require that or mention that.
Okay, so let’s talk a bit about how we approach treatment. We usually use the risk protocol, which I will show you.
Here the standard risk protocol we treat with one placement, kind of sandwiched around the carpal tunnel area. But I’m going to show you a couple of options of how to treat. So the first standard one is taking the array, wrapping it around the carpal tunnel. The first step is a dual red. Of course, it is a continuous wave mode.
This is a stage one for eight minutes, which is a fairly lengthy treatment time at 100% power. That’s followed up by the infrared duo array. It will be modulated using a square waveform. You can see that the frequency and duty cycle are relatively low at 10 Hz cycles per second and 40% duty cycle for ten minutes. Again, a fairly long duration of treatment.
The last step being the infrared probe, the LDI 200. We also use the red probe as well. You can use that if you do have it set to continuous wave for six minutes in and around the area for 40% power. So that would be the typical standard protocol for treating carpal tunnel syndrome. So essentially what I’ve described there is to sort of sandwich the array around the Palmer aspect of the carpal tunnel.
You don’t really need to treat the dorsal aspect because of the bones. You really won’t get any light directly into the carpal tunnel. However, there’s another option that we tend to favor when treating carpal tunnel, and that’s doing two placements. So doing the sandwich approach is a first placement and then doing a parallel approach to try and get a bit more of the actual hand and the thenar region and a bit distal to the carpal tunnel as well, and the median nerve. So we’re going to do the first placement and second placement instead of just this specific wrapping around the carpal tunnel.
So if that’s the case, what we tend to do is use similar parameters. But we’re going to drop down the treatment time of the red to six minutes over the carpal tunnel, then another six minutes in the parallel fashion and then repeat that same placement for the dual infrared at 10 duty cycle. So similar parameters, just two different placements to try and get a bit more of the actual tissue, both proximal and distal the carpal tunnel. So I would already choose the protocols. I would customize the risk protocol and set it up as two places instead of one, and similarly use the LDI 200 probe at 40% power and the red for the same amount of time, 100% power if you do happen to have it.
Moving on to stage two, we’ll start to tweak it a little bit, start to pulse out the dual red at 100 duty cycle and then increase the infrared to 30 80 and increase the power of the LDI 200 to 100% and then sort of increase in that. Stage two, we can increase the frequency of the dual infrared to 50, 80. So we’re still kind of within that stage two boundaries. And then into stage three, you can really start to increase the frequency in the duty cycle of the dual infrared, keeping the other parameters pretty much the same. Okay, so that’s sort of a breakdown of how we might approach using those two placements over several multiple stages of treatment.
Don’t forget, the laser probe should make contact at 90 degrees to the surface to enhance penetration and, of course, minimize reflection. Try to push the probe into the skin to depress the tissue. This allows, again, for the light to go a little bit deeper, a bit more accurate into the actual area that you’re treating. So that’s a really important step to ensure that you’re getting appropriate tissue penetration. As far as the probe itself goes, essentially what you want to do is treat along the path of the median nerve, and then you want to treat and cover the entire carpal tunnel, as well as the thenar eminence and the branches of the median nerve all the way into the first and second finger areas.
Okay, so each time you treat it with the laser probe, you’re going to hold it for 4567, even up to 8 seconds, especially over the carpal tunnel region. You can maybe hold it for a little bit less into the thumb and the fingers, but essentially, you want to make sure you treat the entire carpal tunnel, both proximal and distal into the thumb and the branches and the superficial branches of the median nerve because they, of course, are also affected.
Okay, so as I just mentioned, you want to hold the probe for about five to 8 seconds per point. Once all the points are treated, you can actually go back to the median nerve location in the carpal tunnel and treat. Again, just get a bit of extra dosage in there, but I wouldn’t go back to it more than twice or so. Again, no need to treat the dorsal aspect of the wrist because you’re just going to be irradiating the bones, which won’t get any of that light directly into the carpal tunnel. And again, if you have the LDR 100, it’s also a valuable tool to help with pain and especially the paresthesia in superficial nerves for treating those areas.
A few treatment tips in severe cases. Recall, as I’ve mentioned, they have very poor prognosis. So if a patient’s coming in with muscle atrophy showing really signs of advanced stages of carpal tunnel syndrome, it’s probably not likely to do a lot for the condition because they’re that far advanced. If a patient’s not responding after increasing the parameters, look at treating the cervical spine in stage one with an emphasis on treating the nerve roots of the median nerve, which are C five to T one on the affected side, or bilaterally if they have bilateral carpal tunnel syndrome. We do find that patients respond well to simulation of the origin of the median nerve at the level of a neck when patients just aren’t doing as well as we’d like when treating just local over the carpal tunnel.
So you certainly can add that on to your treatment regime. When treating the carpal tunnel, you don’t have to start off with treating the cervical spine. Usually for mild cases, it’s fine to start at the level of the wrist. However, if you do want to add that on, it would also be helpful. Try and treat the patient consecutively for the first few days, then moving to three times a week, that is every second day, until the patient has made significant improvement, at which point you can start to reduce it to once or twice per week until they’ve achieved maximum medical recovery.
So typically, a treatment plan for mild cases might be ten to 15, moderate cases, 15 to 2025, plus treatments. So you do have to be upfront with your patient. It’s going to take a bit of time. Remember that nerves heal extremely slowly and that you need to be aware of that. Also, you have to address potential underlying causes, whether there are ergonomic issues.
You have to address the use of computers, that kind of thing. Any underlying systemic diseases that need to be treated. All those different things need to be looked at if you’re going to have good clinical results.
Okay, let’s talk a bit about some of the research that I’ve come across with respect to LLLT and carpal tunnel syndrome. This paper was a randomized control trial put out in 2014. It was a double blinded randomized trial. 79 patients with mild to moderate carpal tunnel syndrome.
A lot of the research refers to mild to moderate cases. You will find that it is recommended to treat these cases with LT. However, if it’s a severe case, then chances are they won’t respond very well. And those are cases more that require surgical intervention or more serious types of interventions. This trial used 780 infrared light, 30 milliwatts and a continuous wave.
They treated four points with a contact technique. Each point they held for 90 seconds. So, quite a long time frame. They treated five times a week, once per day for two weeks. So ten treatments in total then every other day for three weeks, for a total of 20 treatments.
Okay, so they were looking at visual analog scale, they were looking at the tinel sign, and they also did neurometrics testing as well for a nerve conduction test. Neurometrics, we use this in our clinic as well too, as a superficial EMG, quite easy to do, gets a result very quickly, almost instantaneously. So if you have the ability to do this or test for it, it really does give objective measurements, pre and post treatment to really get a gauge to see if the motor fibers and the sensory fibers are improving with time and treatment. So they observed that there was significant reduction in pain in this particular trial. There was a reduction in the percentage of patients with the positive tinel sign. And they also found a shortening of the sensory and motor latency with respect to the nerve conduction examination. So overall, they found it quite useful to use LLT with respect to carpal tunnel syndrome.
Another paper published in 2016, so fairly recently they looked at, it was a metal analysis, essentially looking at seven randomized clinical trials. 261 in the control group and 270 in the laser treated group. They concluded that there was improved hand grip, improved bas scale pain, as well as snap testing with respect to functionality of the carpal tunnel.
After three months, a follow up for mild to moderate carpal tunnel syndrome. Again, make note of mild to moderate cases. They did recommend more high quality studies to be done, as most metaanalysis studies require that or mention that.
Okay, so let’s talk a bit about how we approach treatment. We usually use the risk protocol, which I will show you.
Here the standard risk protocol we treat with one placement, kind of sandwiched around the carpal tunnel area. But I’m going to show you a couple of options of how to treat. So the first standard one is taking the array, wrapping it around the carpal tunnel. The first step is a dual red. Of course, it is a continuous wave mode.
This is a stage one for eight minutes, which is a fairly lengthy treatment time at 100% power. That’s followed up by the infrared duo array. It will be modulated using a square waveform. You can see that the frequency and duty cycle are relatively low at 10 Hz cycles per second and 40% duty cycle for ten minutes. Again, a fairly long duration of treatment.
The last step being the infrared probe, the LDI 200. We also use the red probe as well. You can use that if you do have it set to continuous wave for six minutes in and around the area for 40% power. So that would be the typical standard protocol for treating carpal tunnel syndrome. So essentially what I’ve described there is to sort of sandwich the array around the Palmer aspect of the carpal tunnel.
You don’t really need to treat the dorsal aspect because of the bones. You really won’t get any light directly into the carpal tunnel. However, there’s another option that we tend to favor when treating carpal tunnel, and that’s doing two placements. So doing the sandwich approach is a first placement and then doing a parallel approach to try and get a bit more of the actual hand and the thenar region and a bit distal to the carpal tunnel as well, and the median nerve. So we’re going to do the first placement and second placement instead of just this specific wrapping around the carpal tunnel.
So if that’s the case, what we tend to do is use similar parameters. But we’re going to drop down the treatment time of the red to six minutes over the carpal tunnel, then another six minutes in the parallel fashion and then repeat that same placement for the dual infrared at 10 duty cycle. So similar parameters, just two different placements to try and get a bit more of the actual tissue, both proximal and distal the carpal tunnel. So I would already choose the protocols. I would customize the risk protocol and set it up as two places instead of one, and similarly use the LDI 200 probe at 40% power and the red for the same amount of time, 100% power if you do happen to have it.
Moving on to stage two, we’ll start to tweak it a little bit, start to pulse out the dual red at 100 duty cycle and then increase the infrared to 30 80 and increase the power of the LDI 200 to 100% and then sort of increase in that. Stage two, we can increase the frequency of the dual infrared to 50, 80. So we’re still kind of within that stage two boundaries. And then into stage three, you can really start to increase the frequency in the duty cycle of the dual infrared, keeping the other parameters pretty much the same. Okay, so that’s sort of a breakdown of how we might approach using those two placements over several multiple stages of treatment.
Don’t forget, the laser probe should make contact at 90 degrees to the surface to enhance penetration and, of course, minimize reflection. Try to push the probe into the skin to depress the tissue. This allows, again, for the light to go a little bit deeper, a bit more accurate into the actual area that you’re treating. So that’s a really important step to ensure that you’re getting appropriate tissue penetration. As far as the probe itself goes, essentially what you want to do is treat along the path of the median nerve, and then you want to treat and cover the entire carpal tunnel, as well as the thenar eminence and the branches of the median nerve all the way into the first and second finger areas.
Okay, so each time you treat it with the laser probe, you’re going to hold it for 4567, even up to 8 seconds, especially over the carpal tunnel region. You can maybe hold it for a little bit less into the thumb and the fingers, but essentially, you want to make sure you treat the entire carpal tunnel, both proximal and distal into the thumb and the branches and the superficial branches of the median nerve because they, of course, are also affected.
Okay, so as I just mentioned, you want to hold the probe for about five to 8 seconds per point. Once all the points are treated, you can actually go back to the median nerve location in the carpal tunnel and treat. Again, just get a bit of extra dosage in there, but I wouldn’t go back to it more than twice or so. Again, no need to treat the dorsal aspect of the wrist because you’re just going to be irradiating the bones, which won’t get any of that light directly into the carpal tunnel. And again, if you have the LDR 100, it’s also a valuable tool to help with pain and especially the paresthesia in superficial nerves for treating those areas.
A few treatment tips in severe cases. Recall, as I’ve mentioned, they have very poor prognosis. So if a patient’s coming in with muscle atrophy showing really signs of advanced stages of carpal tunnel syndrome, it’s probably not likely to do a lot for the condition because they’re that far advanced. If a patient’s not responding after increasing the parameters, look at treating the cervical spine in stage one with an emphasis on treating the nerve roots of the median nerve, which are C five to T one on the affected side, or bilaterally if they have bilateral carpal tunnel syndrome. We do find that patients respond well to simulation of the origin of the median nerve at the level of a neck when patients just aren’t doing as well as we’d like when treating just local over the carpal tunnel.
So you certainly can add that on to your treatment regime. When treating the carpal tunnel, you don’t have to start off with treating the cervical spine. Usually for mild cases, it’s fine to start at the level of the wrist. However, if you do want to add that on, it would also be helpful. Try and treat the patient consecutively for the first few days, then moving to three times a week, that is every second day, until the patient has made significant improvement, at which point you can start to reduce it to once or twice per week until they’ve achieved maximum medical recovery.
So typically, a treatment plan for mild cases might be ten to 15, moderate cases, 15 to 2025, plus treatments. So you do have to be upfront with your patient. It’s going to take a bit of time. Remember that nerves heal extremely slowly and that you need to be aware of that. Also, you have to address potential underlying causes, whether there are ergonomic issues.
You have to address the use of computers, that kind of thing. Any underlying systemic diseases that need to be treated. All those different things need to be looked at if you’re going to have good clinical results.